A year ago, Mr Djoko, visited my office due to herpetic neuralgia. Sent by prpfesor Adhi Juanda, dermato-venerologyst,. The vesicles already diminished, but his visual analoge scale (v a s) for pain , above 7. Still some hyperpigmentations (spots) area left chest, intercostals space 3,4 , and 5 betwenn sternum and axilla anterior line.
I try to blok the nerve, . two centimeter to the left from body of 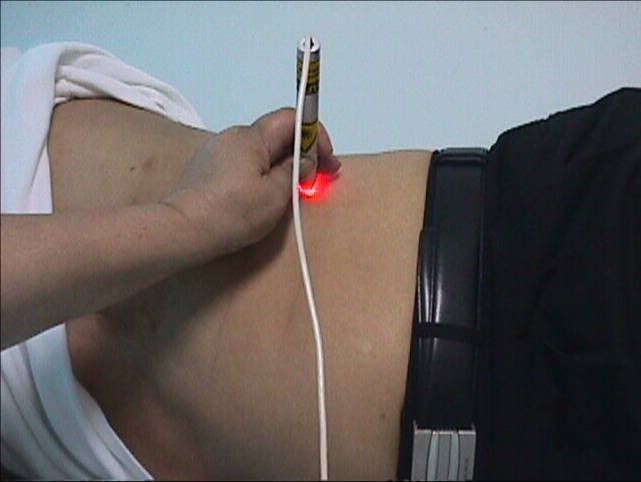 the spine , intercostals 1,2, 3 4 and 5; 5 poiints, 5 Joule per point . same dose at posterior line axillary, and area of spots 3 points, 5 joule every point. The total dose was: 65 Joule. Suddenly after treatment, the vas decreased become 3. (Diode laser 810 nm 50 mW)
the spine , intercostals 1,2, 3 4 and 5; 5 poiints, 5 Joule per point . same dose at posterior line axillary, and area of spots 3 points, 5 joule every point. The total dose was: 65 Joule. Suddenly after treatment, the vas decreased become 3. (Diode laser 810 nm 50 mW)
The pain disappear after 10 treatment (everyday , axept Sunday), but after a week, he felt discomfort again with vas between 3 and 4..
Almost 1 year he come ones a week, with pain vas between 1 - 2.. I give trancutaneus ( half hour), and probe at the points he feel pain, ( 10 minutes). No pain at the end of the the treatment. (Diode 650 nm; transcutaneus 50 mW; probe 50 mW)
 Two months a go, he retired from his office , and begin his own business. He feel more comfort, and the pain no annoying anymore, He still visit my office ones a month, just to make sure no pain again.
Two months a go, he retired from his office , and begin his own business. He feel more comfort, and the pain no annoying anymore, He still visit my office ones a month, just to make sure no pain again.
Discussion:
I used the laser to manage the pain by blocking the nerve. It is not usual for herpetic neuralgia. According to Kert and Rose, they suggest treatment at the vesicle.
Also the dose, rather higher than guidance, they recommend 1 – 2 Joules per point, with total about 15 – 20 Joules.
Is there any connection between the pain and emotional problem ???
Drugs :
Ubi quinon given a long with laser. Ubi quinon works at mitochondria, as well as low laser. Methycobalamin, 500 mg, twice daily. At the first month, drugs for pain also administered.. NSAID, ones a day during first month, after that, he drink, just if the pain going increase more than vas 2.
Here some abstracts :
DOUBLE BLIND CROSSOVER TRIAL OF LOW LEVEL LASER THERAPY (LLLT) IN THE TREATMENT OF POST HERPETIC NEURALGIA
Kevin C Moore MB ChB FRCA Naru Hira. Parswanath Kramer, Copparam Jayakumar & Toshio Ohshiro
Department of Anaesthesia, The
Post herpetic neuralgia can be an extremely painful condition which in many cases proves resistant lo all the accepted forms of treatment. It is frequently most severe in the elderly and may persist for years with no predictable course. This trial was designed as a double blind assessment of the efficacy of low level laser therapy (LLLT) in the relief of the pain of post herpetic neuralgia with patients acting as their own controls. Admission to the trial was limited to patients with established post herpetic neuralgia of at least six months duration and who had shown little or no response to conventional methods of treatment. Measurements of pain intensity and distribution were noted over a period of eight treatments in two groups of patients each of which received four consecutive laser treatments. The results demonstrate a significant reduction in the pain intensity and distribution following a course of low level laser therapy.
Laser Therapy. 1988; 1: 7.
![]()
EFFICACY OF LOW REACTIVE-LEVEL LASER THERAPY (LLLT) FOR PAIN ATTENUATION OF POSTHERPETIC NEURALGIA
Osamu Kemmotsu, Kenichi Sato, Hitoshi Furumido, Koji Harada, Chizuko Takigawa, Sigeo Kaseno, Sho Yokota, Yukari Hanaoka and Takeyasu Yamamura
Department of Anaesthesiology, Hokkaido University School of Medicine, N-15, W-7, Kita-ku,
The efficacy of low reactive-level laser therapy (LLLT) for pain attenuation in patients with postherpetic neuralgia (PHN) was evaluated in 63 patients (25 males, 38 females with an average age of 69 years) managed at our pain clinic over the past 4 years. A double blind assessment of LLLT was also performed in 12 PHN patients. The LLLT system is a gallium aluminium arsenide (GaAlAs) diode laser (830 nm, 60 mW continuous wave) Pain scores (PS) were obtained using a linear analog scale (0 to 10) before and after LLLT. The immediate effect after the initial LLLT was very good (PS: 0-3) in 26, and good (PS: 7-4) in 30 patients. The long-term effect at the end of LLLT (the average number of treatments 36 +/- 12) resulted in no pain (PS: 0) in 12 patients and slight pain (PS: 1-4) in 46 patients. No complications attributable to LLLT occurred. Although a placebo effect was observed, decreases in pain scores and increases of the body surface temperature by LLLT were significantly greater than those that occurred with the placebo treatment. Our results indicate that LLLT is a useful modality for pain attenuation in PHN patients and because LLLT is a non invasive, painless and safe method of therapy, it is well acceptable by patients.
0898-5901/91/020071-05$05.00 Ì 1991 by John Wiley & Sons, Ltd.